|
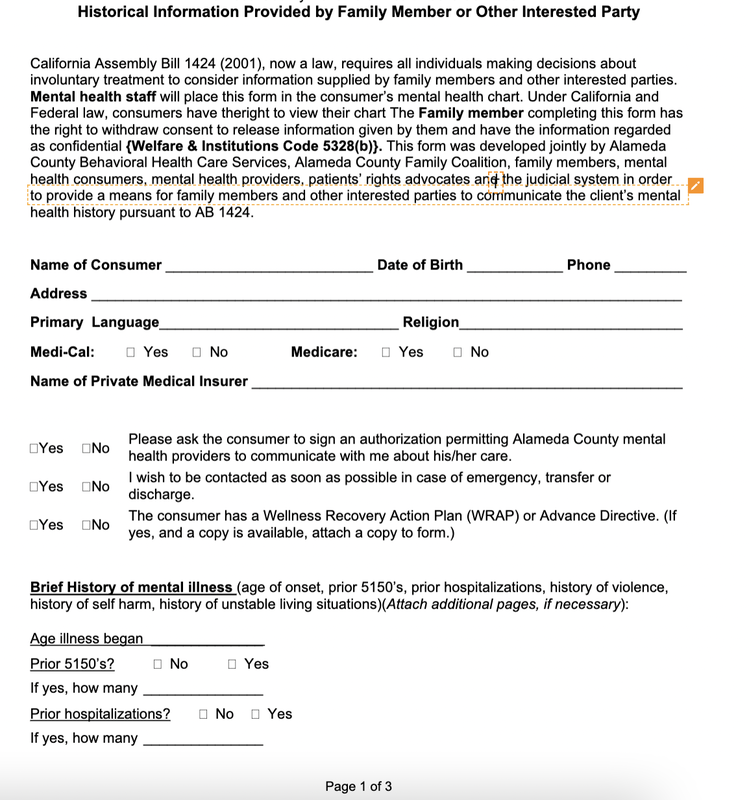
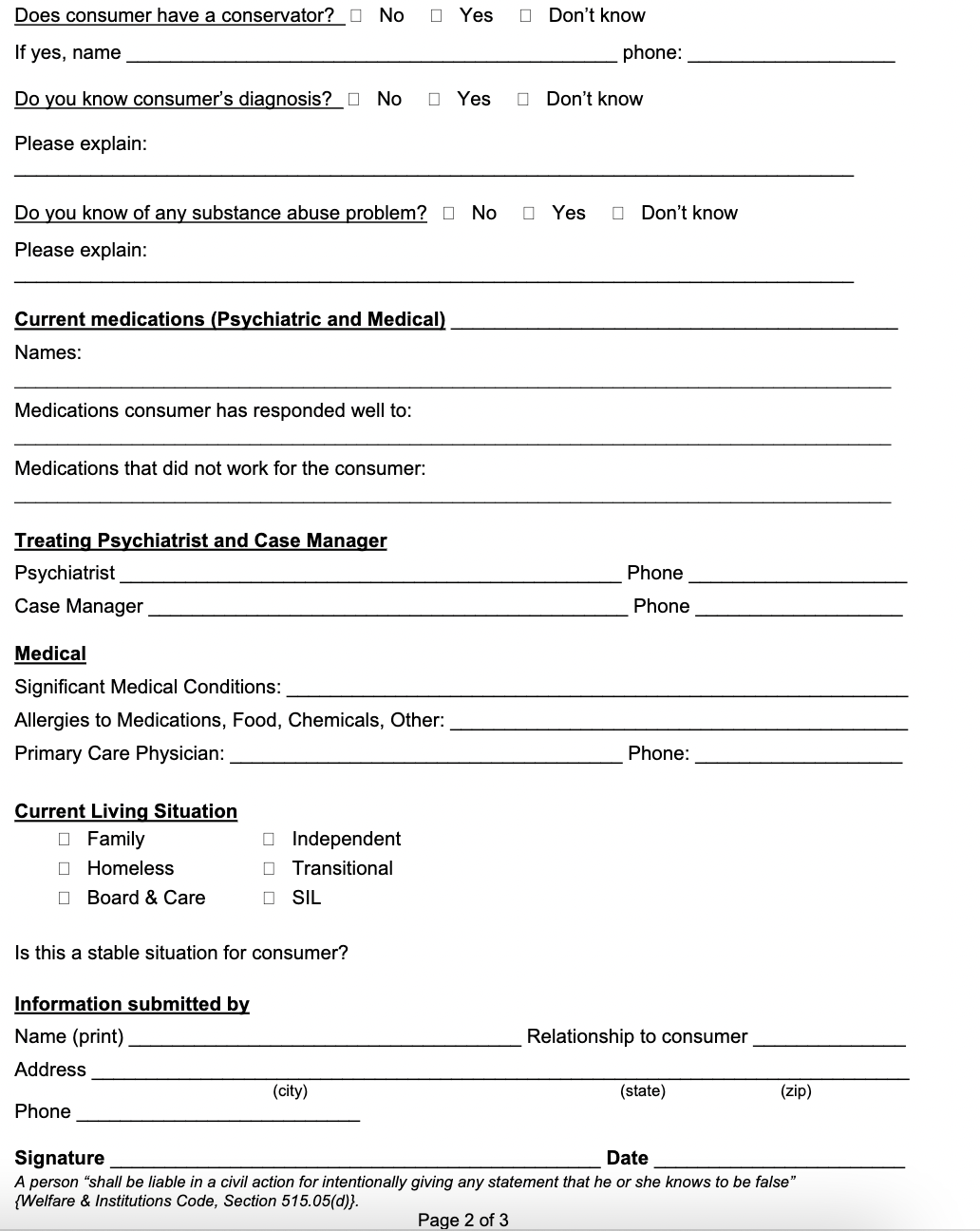
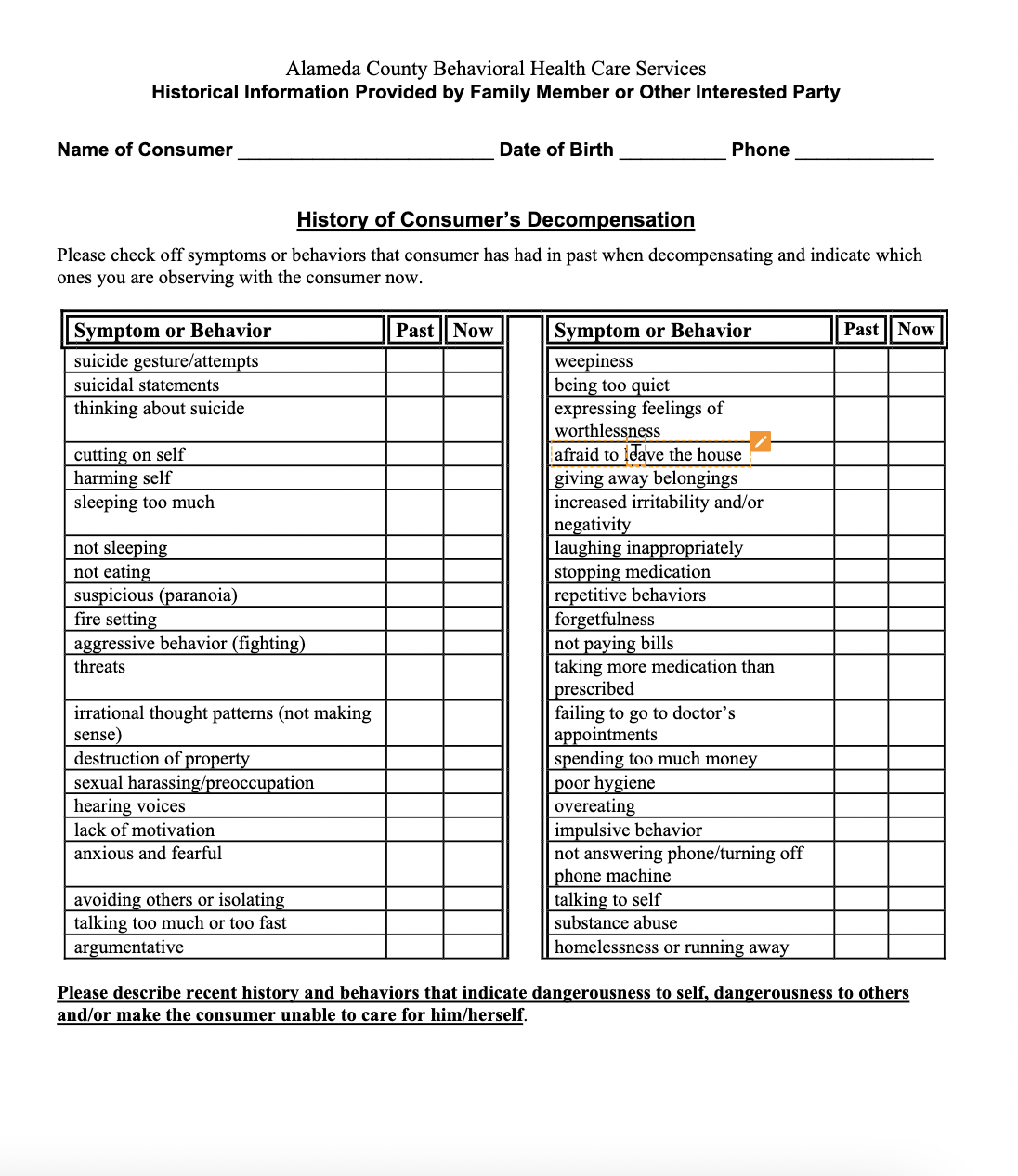
7/24/2021 Assembly Bill 1424 medical history and course of illness during involuntary treatmentRead Now Assembly Bill 1424 or right to consider medical history and course of illness during involuntary treatment On October 4, 2001 Assembly Bill 1424, the right to have input and medical history considered when making a determination of whether a patient is a danger to self, others, or gravely disabled, was codified into Welfare Inst Code and became effective Jan. 1, 2002. However, hospitals and police officers routinely do not remember that this has been codified or ignore this making obtaining involuntary treatment much more difficult. The proposal states: "The Legislature finds and declares all of the following: Many families of persons with serious mental illness find the Lanterman-Petris-Short Act system difficult to access and not supportive of family information regarding history and symptoms. Persons with mental illness are best served in a system of care that supports and acknowledges the role of the family, including parents, children, spouses, significant others, and consumer identified natural resource systems. It is the intent of the Legislature that the Lanternman-Petris-Short Act system procedures be clarified to ensure that families are a part of the system response, subject to the rules of evidence and court procedures." In simpler terms it allows for the peace officer or the mental health provider to: consider the historical course of the person's mental illness if has a direct bearing on danger to self/others or gravely disability relevant evidence via medical records or presented orally or written form by family members, treatment providers be considered by the court in determining the historical course of illness and that the treating facilities make reasonable efforts to ensure that information provided by relatives and others are available to the court This has been codified in several sections of Welf & I C such as § 5150.05 now added to Welf & I C § 5150. When determining if probable cause exists to take a person into custody, or cause a person to be taken into custody, pursuant to Section 5150, any person who is authorized to take that person, or cause that person to be taken, into custody pursuant to that section shall consider available relevant information about the historical course of the person's mental disorder if the authorized person determines that the i.nformation has a reasonable bearing on the determination as to whether the person is a danger to' others, or to himself or herself, or is gravely disabled as a result of the mental disorder. Working with Mental Health Providers when it comes to Grave disability or Danger to Self/Others Generally when working with hospitals it will be very hard to get them to take your information. Workers and providers will defer to HIPAA when asked about taking in evidence. It takes a lot of pushing and reminders. It is wise for caretakers to print several copies of their record and then provide that to three different persons. The hospital often has a fax or email those providers can use. It is wise to email or fax the social worker assigned to the case, the charge nurse asking that they be to attach to the patient’s file, and in smaller hospitals, the psychiatrist. The caretaker must be diligent and ask and make several calls to get the names and emails of those persons. It can be frustrating and draining but due to all the red tape there is no other way. Strong wording is often required when convincing social workers of the law and what is allowed in records and now. For example, the following wording has been used to convince a hospital to allow out of court family statements in a cert review hearing: The court must consider the "historical course" of the patient’s mental disorder when applying the definition of mental disorder s (in re Azzarella, 207 Cal. App. 3d 1240 Ct. App. 1989; Welf & I C §5008.2. Because of this we are asking that the court consider the patient’s history of repeated noncompliance and devolvement into psychosis and grave disability as equally important factors in determining his ongoing grave disability. We are asking that the court consider these following statements alongside the hospital records and other submitted photographic and written evidence in rendering a judgement whether patient is gravely disabled by a preponderance of the evidence and in need of further detainment and treatment. Likewise the same has been done for LPS Conservatorship court investigation reports when family members struggled to have certain documents submitted into the CIR for the P-con date. Similar documents needed to be produced reminding the county of the law and right to have evidence considered in an uncontested LPS Conservatorship bench hearing. In the matter of Conservatee HEARSAY EXCEPTION IN COURT INVESTIGATION REPORT I respectfully submit further information to supplement the court investigator’s report in the matter of permanent conservatorship of Conservatee. The statements in this report should be deemed admissible given that this matter current is not a contested trial. In re Conservatorship of Manton (1985) 39 C3d 645: An LPS conservatorship investigation report containing hearsay statements from doctors, relatives, and other third parties can be admitted at a hearing; to the extent that the report contains inadmissible hearsay, however, it cannot be admitted into evidence in a contested trial on the issue of whether the person is gravely disabled. Should county counsel find that these statements are inadmissible, then the public conservator investigator has the power and authority to subpoena the necessary evidence and authenticate the following records to ensure that they comport with evidentiary requirements under Manton. A final note: This has been stated by advocacy groups but not always honored by many hospitals: California law requires that hospitals inform families that a patient has been admitted, transferred, or discharged unless the patient requests that the family not be notified. Hospitals are required to notify patients they have the right not to provide this information. Although the hospital health providers are constrained in their ability to communicate with families, family members may communicate with treatment teams with or without authorization. This means that family members can be allowed to relay information about their loved one but they will not be told anything about their relative’s status. Sample forms below Personalized letters with more specific symptoms, nexus to GD, DS, DO, and citations to legal authority are preferred as they sound more formal and are more thorough. However, these forms are a good starting point for caretakers who do not have much time on their hands.
0 Comments
Leave a Reply. |
Details
Juvenile Dependency and
|