WRAPPING IT ALL TOGETHER AND CREATING THE NEXUS BETWEEN SYMPTOMS, HISTORY, COMPLIANCE, THIRD PARTY ASSISTANCE TO PROOF OF CURRENT GRAVE DISABILITY BEYOND A REASONABLE DOUBT (WIP)
As you can see with the list below, it lists the symptoms and the facts that the patient is unable to food, clothe, or provide shelter for himself. However, there lacks a clear nexus and deference to the law. The list has what symptoms the patient is having but law enforcement or the hospital will find the holes between these symptoms and current grave disability. There needs to be a report that does not leave any gap for guessing or conclusions. After the sample report generously borrowed from Bet Tzedek's LPS handbook, there is a longer more comprehensive symptom list and the nexus between grave disability.
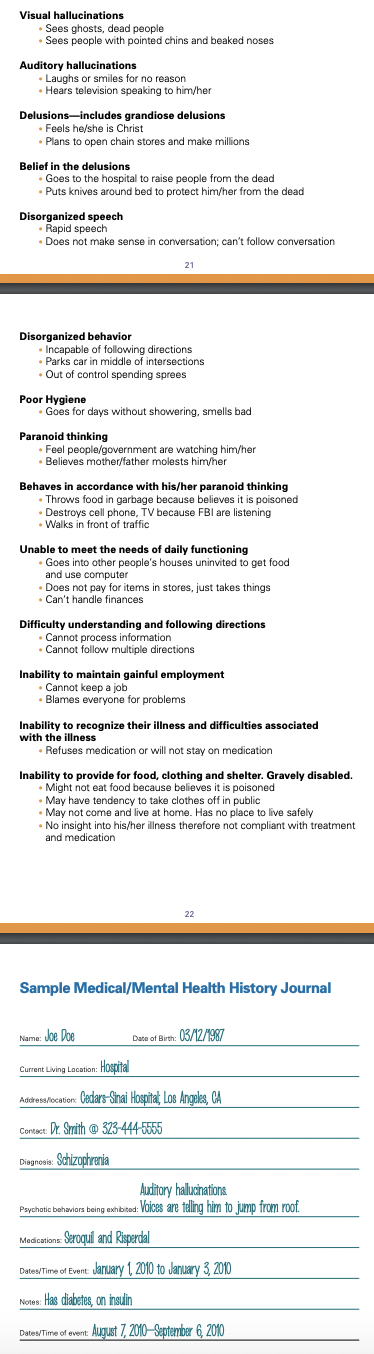
Short List for Quick Evaluation for 5150
This example is for a patient who refuses to eat food and is gravely disabled as a result and needs 5150 evaluation at a LPS designated facility. A longer more complete evaluation samples is in the next section for LPS Conservatorship petitions.
Current Psychiatric Symptom
How it causes impairment with getting proper food
Patient is too ill to accept meaningful third party assistance in getting his needs of food met
How his impairment would constitute grave disability
This example is for a patient who refuses to eat food and is gravely disabled as a result and needs 5150 evaluation at a LPS designated facility. A longer more complete evaluation samples is in the next section for LPS Conservatorship petitions.
Current Psychiatric Symptom
- Patient suffers from delusions that his food is bad or poisoned
- He believes others are engaged in a plan to harm him or kill him
- He believes this for days/weeks at a time
- He becomes very agitated during these episodes and yells at people
- He refuses to take any medication IM or oral meds to help stop the delusions
- He lacks the insight into his _____ illness and the need for meds for such illness
How it causes impairment with getting proper food
- Due to his lack of insight into ______ illness and refusal to take meds his delusions persist for weeks to months
- Because of his delusion that his food is poisoned he will not accept food from others
- He becomes internally preoccupied due to his untreated delusions and does not have the cognitive clarity to take time to prepare and eat a proper meal
- Because he refuses to eat a meal, he has lost ___ pounds in the last 6 months
- He cannot recognize his basic need for healthy nutrition and does not understand the dangers of being low weight
- When asked about his insight into this problem, he avoids the question or talks about his delusion citing it as the reason for his refusal to eat
- He cannot formulate a plan of care should he become very ill due to malnutrition
Patient is too ill to accept meaningful third party assistance in getting his needs of food met
- Caregiver can no longer help provide patient as he is too internally preoccupied with his delusions and agitation that he persecutes, insults, threatens, and yells at his support network
- His illness is too severe for any reasonable healthy person to intervene and help him meet his needs of food
- No one family members or professionals can help talk him out of the delusion
- He refuses anyone to help him with food as he believes that they are part of a plan to harm him
How his impairment would constitute grave disability
- With these severe ___ symptoms he can’t properly assess his abilities to use resources or balance the risks & benefits of not eating
- Therefor he truly lacks capacity to make an informed decision
- He is gravely disabled as in he cannot provide for his own need of food and suffers health consequences as a result such as low BMI, ____, and _______.
- Only one criterion of food, clothing, or shelter needs to be met for a finding of grave disability in re Conservatorship of Carol K. (2010) 188 CA 4th 123, 135
- Therefore his inability to provide food, one of the three criteria, should be enough to trigger the need to transport him to a LPS designated facility for evaluation.
LPS conservatorship summary and report
Note how each section details symptoms and then ties it into meeting criteria for current grave disability and then refers to Welfare and Institutions Code for legal authority.
SUMMARY OF HISTORY OF PSYCHIATRIC TREATMENT
HOSPITALIZATIONS-
The court may consider the patient’s "historical course" of the proposed conservatee's mental disorder must be considered if it directly bears on the determination of whether the person is gravely disabled. Welf & I C §5008.2
- Hospitalized ____ times for involuntary inpatient psychiatric care during young adulthood
- Hospitalized in date at hospital in ____. Diagnosed with bipolar affective disorder. Discharged to home of relative. Decompensation after four months of medication noncompliance and escalating psychotic behaviours.
- Hospitalized in date at hospital in ____. Involuntary hold. Diagnosed with depression and psychosis. Held until 14 day hold expired. Discharged once more to home of relative with orders for outpatient therapy and psychiatric care. Discharged to home of relative. Decompensation again due to psychosis and inability to take care of ADLs due preoccupation with voices and delusions. Refused medication due to believing that he did not have a mental illness. Refused outpatient therapy or treatment with psychiatrist.
- Hospitalized in date at hospital in ____. Involuntary hold. Diagnosed with depression and psychosis. Currently being held on a ______ hour hold.
SUMMARY OF GRAVE DISABILITY SYMPTOMS-
a person, as a result of a mental health disorder, is unable to provide for his or her basic personal needs for food, clothing, or shelter Welf & I C § 5008 (h)
ONLY ONE OF THE THREE IS NEEDED FOR A FINDING OF GRAVE DISABILITY-
“grave disability can be determined on an inability to provide for food, clothing, or shelter”. It does not require a finding that a proposed LPS Conservatee cannot provide for his food, clothing, and shelter” Conservatorship of Carol K. (2010) 188 CA 4th 123, 135
INABILITY TO PROVIDE FOR SHELTER
- Patient is currently without a home, an apartment, or men’s shelter to return if discharged
- Patient is unable to provide for this basic need of shelter because his psychosis and delusions render him unable to understand the importance of maintaining shelter or going through the necessary steps to secure housing.
- Patient prior to admission and currently presents with symptoms of delusions of controlled by the devil and religious persecution. These delusions render patient verbally and physically aggressive as he believes that his relative and others are out to hurt him and are agents of the devil. Because of these fixed beliefs, he refuses to obtain medication as it represents giving into the devil and other agents of chaos, and as a result his psychotic aggression escalates marking him too risky to be a resident in a shelter or a tenant at an apartment.
- Because of his psychotically driven delusions, he threatens his mother who is providing means for his residence. He believes that she is trying to poison him with medication and refuses to comply with her contact that he be med compliant to live at home. Without insight into his illness and a willingness to take medication she opines that his mental illness is too severe to be managed on an in-home basis and is no longer willing to provide a home for him.
- Information, resources, and contacts have been offered to the patient about how to secure affordable housing or to find placement in a men’s shelter, but again due to his limited insight and delusions he is unable to avail himself of these emergency shelter opportunities.
- When offered to be driven to a men’s shelter, he decompensated yelling, threatening, and accusing the relative and intake staff at the shelter that they are out to harm him and he will not comply with their “plans to hurt and control him”. Staff have informed and provided reasonable rules as to how patient must comport himself when on the premises, but Patient’s psychosis and delusions of persecution render him unable to understand and accept that their rules are reasonable and not a show of violence.
- He refuses to act in a safe, legal, and respectful manner thus marking him as a liability to any men’s shelter thus rendering that option untenable without forced psychiatric care.
- Similarly, Patient has many times voiced his concern and fear that people in public such as strangers and other homeless people are “bad people” who will hurt him, rob him of any money, and are agents of the devil. Given his proclivity to act in an aggressive and disruptive manner toward those whom he believes are out to harm him, even if Patient were to be live among the homeless in an encampment, his psychotic aggression would lead to dangerous fights and expulsion as he would place his and others’ safety at risk. He has never lived with strangers before and placing him in their care would lead to immediate life threatening consequences.
- Patient has never earned any form of substantial income in his life. His psychotic processes and inability to see which behaviors are acceptable make him unable to sustain any form of employment and earn any kind of income. historically he has lived off money from relatives but due to his refusal to take medication or behave in a safe appropriate manner, relatives opine they are unable to offer financial support at this time.
INABILITY TO PROVIDE FOR SHELTER
- Patient is unable to provide for his food by either himself or through the assistance of third party assistance.
- Patient believes that other members of his household such as his relative are evil persons intent on harming him and consequently believes that they are poisoning the food he eats.
- As a result, he refuses to eat any of the food they offer him or refuses to allow them to go out and buy food ingredients to cook at home.
- Because he refuses to take any medication, he suffers delusions that impede his ability to plan and put together a cohesive plan to cook a basic meal. His delusions of persecution occupy his thoughts every day which leads to this internal preoccupation that prevents him from remembering to buy fresh new ingredients for food or to throw out old food.
- He eats old expired scraps when he does choose to eat which places him at risk of becoming ill from food poisoning.
- In the same vein, he believes that others are bad persons who will cause him harm and refuses to go to a soup kitchen or food pantry to obtain the ingredients himself thus leaving him with no real sustenance.
- He has lost x pounds in the last three months due to his refusal to eat an appropriate amount of calories. He is at risk of dehydration and malnutrition from a consistent refusal and misdirected fear of food and those who can help with food.
- Should he suffer severe health complications from a refusal to eat, his internal preoccupations with his delusions and aggressive behaviour prevent him from seeking life saving medical care. He has no relatives or friends who be able to help should he suffer from this kind of medical emergency.
- When Patient’s behaviour escalates into extreme paranoid delusions of grandeur, he believes that he is enlightened and does not need any form of food to survive. He believes that spirits will help keep him healthy and refuses any kind of personal or medical intervention to provide calories.
- If the hospital chooses to discharge him, he will return to refusing meds heralding back an inevitable return of psychosis and delusions of persecution which will lead him to not trust anyone with food assistance and a belief he does not need basic nutrients to survive thus precipitating dangerous weight loss and dehydration.
INABILITY TO PROVIDE FOR CLOTHING
- Patient’s daily preoccupation with spirits and evil people distract him from being able to keep his body and clothes clean.
- Patient believes that he must fight evil presences and work with spirits in his body before he can address the very important issue of taking care of his physical hygiene and clothing.
- When asked to change his clothes, do laundry, or wash his body with soap, patient becomes verbally and sometimes physically aggressive stating that he does not want to be bothered by the chore of cleaning and showering. His misdirected anger and aggression make the simple task of helping or reminding about personal hygiene impossible and dangerous for third party persons to aid in safely.
- His delusions of persecution and internal preoccupation with these delusions are a daily ongoing deterrent as he regularly refuses to take his medication or engage in outpatient therapy, so as a result his hygiene is consistently poor.
- He does not change his clothes and leaves them in a malodorous pile in his room making them and himself smell poorly.
- He does not use any money offered to buy new clean clothes or go clean the ones he has.
- He sleeps in very dirty clothes with dirt and food all over them. He runs a high risk of developing some form of dangerous skin infections or severe rashes as a result.
- Without forced stabilization on medication regimen and strict enforcement by skilled nursing staff, he is unable to provide for his basic need of proper hygiene.
- Should he be discharged, he will return to medication noncompliance, a inevitable return of his psychotic and delusional thinking, and stop caring for any aspect of his personal hygiene.
LACK OF SAFE AND EFFECTIVE THIRD PARTY ASSISTANCE-
Even if a third party offers assistance, the court may still determine that the assistance offered, though well-intentioned, is not sufficient to permit the conservatee to survive safely… and [that] the conservatee's condition is so severe [that] it is "beyond an ordinary person's ability to deal with" Conservatorship of Jesse G. (2016) 248 CA4th 453, Conservatorship of Johnson, 235 CA3d at 698
- Patient has no safe effective third party assistance to help him find and keep his shelter/housing as his disruptive, aggressive, rude, and demanding psychotic behaviour has alienated himself from any friends or family.
- Because his primary presenting symptom is a regular delusions of persecution, he frequently devolves into yelling, threatening, and accusing those who offer assistance with food, clothing, and shelter.
- He makes threats of harming them, stating he does not want their assistance, or simply isolating himself in his room out of fear that they will harm him or poison his food toward those who are trying to provide for his care.
- When approached by relatives or friends about taking medication to reduce his symptomology in order to make the process of helping him more reasonable, he yells and shouts that his medication is a poison and he does not need it. Because of his refusal to take medication, his psychotic delusions persist, rendering any offer of help unappreciated and a dangerous endeavor.
- He is unable to panhandle on the street as he frequently complains that others are also complicit in this plan to harm him thus it would apply that that he would be aggressive toward others in his panhandling efforts thus making it unsuccessful.
FAMILY MEMBERS WILLING TO OFFER ASSISTANCE-
Unless family, friends, and others specifically indicate in writing their willingness and ability to help, however, they must not be considered willing and able to provide this help. Welf & I C §5350(e)(2)
- Patient has no family members who are willing to help with food clothing or shelter due to his abusive behavior and psychosis.
- His relative refuses to send any money to aid with housing or food as she opines that he is too disorganized and preoccupied with his delusions of persecution to properly understand how to spend his money on necessities.
- He has no friends to rely on to send money to support him or provide safe housing.
- The relative has submitted a personal statement that she is unwilling to provide assistance, why she finds herself unable to, and her experiences that lead her to believe that without her assistance he will be unable to survive.
- This statement can be found in an attachment.
- There are no statements by Patient’s known associates stating that they are willing to aid.
ADDITIONAL FACTORS OF INSIGHT INTO ILLNESS, MED COMPLIANCE, AND WILLINGNESS TO COMPLY-
Although a finding that the proposed conservatee is unable or unwilling to accept treatment is not a prerequisite to establishing an LPS conservatorship but along with evidence that the proposed conservatee lacks insight into his mental illness, does not believe he needs medication, will not take medication without enforcement, and as a result will be unable to provide for his or her own basic needs, may be sufficient evidence to establish an LPS conservatorship- (Conservatorship of Guerrero (1999) 69 CA4th 442), (Conservatorship of Walker (1989) 206 CA3d 1572). (Conservatorship of Symington (1989) 209 CA3d 1464)
PATIENT HAS BEEN ADVISED OF THE NEED FOR MEDICATION BUT IS UNABLE OR UNWILLING TO ACCEPT TREATMENT ON A VOLUNTARY BASIS
- Patient when discharged from the hospital upon his first discharge in year stated that he did not believe that he needed medication and that his decompensation was a result of personal life issues.
- He was offered information about his diagnosis, the biological basis and recurrent nature of the symptoms, the consequences of refusing medication, and the high risk of rehospitalization due to recurrent psychosis.
- He was also offered outpatient psychiatric care and medication management at a reasonable location and via proper coverage.
- Despite all of this information being provided to patient in an accessible manner, he refused to take his medication citing that he (1) did not have a mental illness nor did he need the medication (2) and later that the medication was poison or dangerous to his body despite plenty of proper authority citing its safety.
- During his subsequent decompensations and hospitalizations, he was proffered the same information and refused providing the same reasons.
- Even when at home with relative, he refused to see an outpatient psychiatrist or to pick up his medication for the same reasons.
- Even when offered a ride and means of payment for the medication, he did not trust the doctor or his caretaker to not “poison” or “control him” through medication.
- Patient only takes his medication as prescribed when offered in the setting of an involuntary inpatient milieu as his involuntary legal status allows nursing staff to override his psychotically based objections, provide temporary stabilization that allows him partial degree of insight into his condition, and thus making the process of accepting medication a degree easier.
- When discharged, he no longer is under the power of the involuntary laws that allow for forced medication and the resulting temporary stabilization on a locked unit thus making outpatient med management an impossible reality due to its voluntary nature.
- Patient has been informed many times of what his diagnosis is and the need for medication but because he does not face involuntary care once discharged, he refuses to seek proper consistent treatment for his psychosis.
- When asked to go to the clinic or offered assistance to go treat his mental illness he does not follow up and states that he does not have a mental illness and that he has been cured.
- Patient has been provided details on what his behaviour was like when he is unmedicated and that his illness is responsible for his inability to provide for his basic needs, but he lacks insight to truly absorb this information due to his relatively short period of being medicated to a point of lucidity.
PATIENT ONLY TAKES MEDICATION REGULARLY WHEN HE IS SUPERVISED ON A LOCKED UNIT WITH AN INVOLUNATARY MEDICATION ORDER
- Patient only takes his medication when he is supervised in a locked setting.
- To achieve this, patient has had three Riese petitions granted as he was noncompliant on his involuntary holds.
- Patient’s symptoms stabilize when he is medicated on the unit and his delusions of persecution and grandeur decrease enough to where he can listen, engage, and work to make changes in how he approaches compliance with outpatient treatment.
- However any superficial stability is only maintained and achieved through strict observation and involuntary medication orders and rapid decompensation once discharged has been demonstrated through his repeat hospitalizations through the years of ______ and ______.
- Neither patient’s family nor friends can get him to take his medication when not in a locked unit as he will escalate with verbal threats or statements about delusions of persecution making the task of aiding with medication management impossible.
- He will not consent to a long acting injection on the unit thus making lasting stabilization post discharge impossible.